Bipolar disorder generally requires lifelong medication. Today, second generation antipsychotics (SGA) are sometimes used for maintenance treatment, either as monotherapy or in combination with lithium or other mood stabilisers.
SGA is prescribed in relatively high numbers of cases of bipolar disorder. According to The Swedish National Quality Register for Bipolar Disorder, a combination of SGA and mood stabilisers was prescribed in 2014 for 20% of all patients registered for follow-up, but SGA was prescribed as monotherapy for only a very small percent.
The purpose of this project is to evaluate the benefits and risks of maintenance treatment of bipolar disorder with SGA (of at least six months’ duration), with special reference to medical, ethical and health economic perspectives.
Conclusions
In the long-term
- As there are no studies of more than two years’ duration, it is not possible to assess the long-term benefits and risks of SGA for maintenance treatment of bipolar disorder.
In the short-term
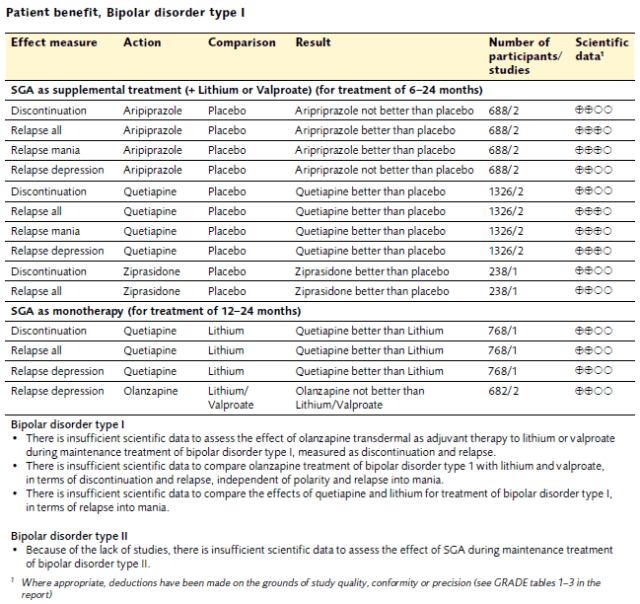
Bipolar disorder type I
- For patients with bipolar disorder type I who have responded to aripiprazole, quetiapine or ziprasidone as adjunct to mood stabilisers in the manic acute phase, the risk of relapse is reduced when these drugs are used during maintenance.
- There is insufficient quality of studies in order to evaluate the effects of maintenance treatment using olanzapine and risperidone.
- In some patients, quetiapine could be an alternative to lithium for reducing the risks of relapse and treatment discontinuation. While the risk of serious side effects must be considered, to date no long term studies are available.
- Weight gain is frequently associated with all of the SGA investigated. Aripiprazole causes slightly more tremors and tingling in the legs than mood stabilisers. Olanzapine and quetiapine are associated with more daytime drowsiness and less insomnia than mood stabilisers. It is a requirement that side effects are reported to the Medical Products Agency and should be followed up in quality registers.
- Drugs which prevent relapses have the potential to redeem much of their cost by reducing the healthcare costs associated with relapses. Fewer relapses improve quality of life and survival.
Bipolar disorder type II
- In the absence of studies, no conclusions can be drawn about the effect of SGA as maintenance treatment for bipolar disorder type II.
Economic aspects
The annual cost per patient of medication with SGA is around SEK 700 for quetiapin and around SEK 16 000 for aripiprazol. The patent for aripiprazol expired recently and the price will probably drop as generic alternatives become commercially available. However, whether SGA treatment can be considered to be good use of resources, compared with either mood-stabilising pharmaceuticals alone or in conjunction with SGA, depends primarily on the effectiveness of SGA drugs in reducing the number of manic and depressive relapses. Fewer relapses are associated with better quality of life, increased survival rates and reduced societal costs. SGA which are effective in preventing relapses have the potential to save a considerable amount of the cost of the medication by reducing the health and medical costs associated with relapse. Assessment of the cost-effectiveness of the methods should however, also take into account the influence of the medication on costs and quality of life and the consequences of side effects.
Ethical aspects
Only limited information is available about the long-term effects and side effects of antipsychotic drugs. It is therefore important that currently available information about side effects is factual and objective and that the psychiatrist, in consultation with the patient, assesses whether the risk of side effects is outweighed by the anticipated benefits of the treatment. Periods of illness cause a reduction in functional level and quality of life and can lead to compulsory admission for institutional care, which is a major uppheaval for both the patient and close relatives. Because of the sporadic nature of the illness, conflict may arise between patient and healthcare personnel as to the need for maintenance treatment. This is particularly obvious under periods of neutral or slightly elevated moods when the patient feels well, but his/her decision-making capacity may be impaired. Healthcare professionals may then be tempted ”in the best interests of the patient” to try to force or at least to influence the patient to continue medication against their will. This could then be perceived as a conflict between the obligation under the Health and Medical Services Act for the health services to achieve good health and quality of life for the patient and the patient’s rights, according to the legislation, requiring informed consent for treatment.
Patient benefit, Bipolar disorder type 1